Vital Neuroblastoma projects we fund with your donations
Collaborating to find a cure
Earlier this year, Niamh’s Next Step joined forces with childhood cancer charities Neuroblastoma UK and The Bradley Lowery Foundation to fund more vital research into neuroblastoma.
Dr Juliet Gray is Associate Professor in Paediatric Oncology at the University of Southampton. Together, the three charities are funding her vital work into antibody immunotherapy for children with neuroblastoma, a form of treatment which relies on cells of the body’s own immune system to kill cancer cells.
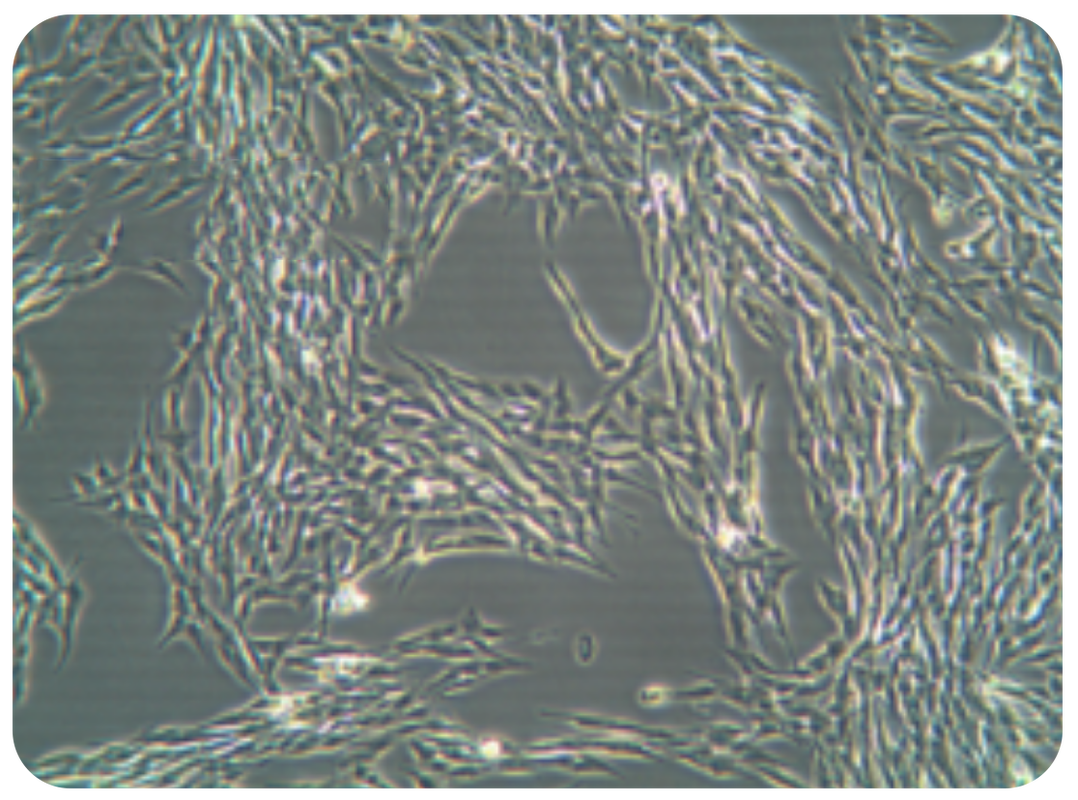
Dr Gray says “As lead investigator, I am working with my team on a clinical trial to understand and improve the effectiveness of anti-GD2 immunotherapy in neuroblastoma. The antibody acts against a sugar-fat molecule present on nearly all neuroblastoma cells called GD2 (disialoganglioside). When the antibody binds to GD2 on the neuroblastoma cells, the cells die in a different way than after chemotherapy or radiotherapy. This is called antibody dependent cytotoxicity.
“The introduction of immunotherapy with anti-GD2 antibody has seen improvements in the outcome of children with neuroblastoma and has become an international standard of care. However although early relapse rates are significantly reduced, long term benefits are less clear, suggesting that, in many children, relapse is delayed rather than prevented.
Furthermore, side effects from anti-GD2 are significant, with many children still developing severe pain and central nerve damage, such as paralysis. The majority of children with high risk neuroblastoma still die from their disease.
THE AIMS OF THE RESEARCH PROJECT
“The first aim of the project is to design a better anti-GD2 antibody that will be more effective in killing the neuroblastoma cells and less toxic than those which are currently used, to reduce the serious side effects of treatment.
If this project is successful, it would hopefully lead to the subsequent development of a clinical antibody, for trial in children. Ultimately it is hoped such an antibody would be result in less pain and neurotoxicity for children than current antibodies, and also help cure more children.
...If this project is successful, it would hopefully lead to the subsequent development of a clinical antibody, for trial in children with neuroblastoma…
“The project will also investigate if anti-GD2 therapy can be further improved by combining with two different agents (anti-PD-1 antibody and STING agonists) to stimulate the immune system and increase response to treatment.
Both of these agents are already in clinical trial, and therefore successful pre-clinical combinational strategies with anti-GD2 could be rapidly translated into clinical trial for children with neuroblastoma. Such trials would aim to improve the efficacy of anti-GD2 therapy, curing more children.
...Ultimately it is hoped such an antibody would be result in less pain and neurotoxicity for children than current antibodies, and also help cure more children with neuroblastoma…
“My motivation for research and new clinical trials comes from the patients that I see, and the need to find new and better treatments for the cancers that they have. New and different types of therapy are needed to improve survival rates for children with neuroblastoma. Anti-GD2 immunotherapy has already been shown to improve survival for these children, but there is still a lot of work to be done to improve survival rates further.
“Thanks to funding from Niamh’s Next Step, Neuroblastoma UK, and The Bradley Lowery Foundation, I hope the trials I am involved in can build on what has already been achieved, and deliver more effective immunotherapies.”
Funding research. Giving hope.
Tony Heddon, Chair of Neuroblastoma UK says, “Thanks to our generous supporters, we have awarded nearly £7 million to UK research focusing on neuroblastoma. But more needs to be done. We rely on donations to continue to drive forward research into this terrible disease and give more families hope.”
Chris Curry, Niamh’s dad, Co-Founder and Chair of Niamh’s Next Step says, “Having collaborated on various neuroblastoma research projects over the last six years, we are very proud and excited to be working alongside Neuroblastoma UK and The Bradley Lowery Foundation to fund this project run by Dr Gray in Southampton. It’s amazing to continue funding vital projects like this in Niamh’s memory.”
Gemma Lowery, Bradley’s mum and founder of The Bradley Lowery Foundation says, “The Bradley Lowery Foundation believe collaborating with other like-minded charities and organisations is the best way to achieve the goals you desire. Working with so many great charities, we have been able to support vital research into neuroblastoma, in the hope that one day, it can be cured for good. BLF are honoured to join Neuroblastoma UK and Niamh’s Next Step in funding this research and we believe, together, great things can be achieved.’’
Dr Juliet Gray is Associate Professor in Paediatric Oncology at the University of Southampton. Together, the three charities are funding her vital work into antibody immunotherapy for children with neuroblastoma, a form of treatment which relies on cells of the body’s own immune system to kill cancer cells.
Dr Gray says “As lead investigator, I am working with my team on a clinical trial to understand and improve the effectiveness of anti-GD2 immunotherapy in neuroblastoma. The antibody acts against a sugar-fat molecule present on nearly all neuroblastoma cells called GD2 (disialoganglioside). When the antibody binds to GD2 on the neuroblastoma cells, the cells die in a different way than after chemotherapy or radiotherapy. This is called antibody dependent cytotoxicity.
“The introduction of immunotherapy with anti-GD2 antibody has seen improvements in the outcome of children with neuroblastoma and has become an international standard of care. However although early relapse rates are significantly reduced, long term benefits are less clear, suggesting that, in many children, relapse is delayed rather than prevented.
Furthermore, side effects from anti-GD2 are significant, with many children still developing severe pain and central nerve damage, such as paralysis. The majority of children with high risk neuroblastoma still die from their disease.
THE AIMS OF THE RESEARCH PROJECT
“The first aim of the project is to design a better anti-GD2 antibody that will be more effective in killing the neuroblastoma cells and less toxic than those which are currently used, to reduce the serious side effects of treatment.
If this project is successful, it would hopefully lead to the subsequent development of a clinical antibody, for trial in children. Ultimately it is hoped such an antibody would be result in less pain and neurotoxicity for children than current antibodies, and also help cure more children.
...If this project is successful, it would hopefully lead to the subsequent development of a clinical antibody, for trial in children with neuroblastoma…
“The project will also investigate if anti-GD2 therapy can be further improved by combining with two different agents (anti-PD-1 antibody and STING agonists) to stimulate the immune system and increase response to treatment.
Both of these agents are already in clinical trial, and therefore successful pre-clinical combinational strategies with anti-GD2 could be rapidly translated into clinical trial for children with neuroblastoma. Such trials would aim to improve the efficacy of anti-GD2 therapy, curing more children.
...Ultimately it is hoped such an antibody would be result in less pain and neurotoxicity for children than current antibodies, and also help cure more children with neuroblastoma…
“My motivation for research and new clinical trials comes from the patients that I see, and the need to find new and better treatments for the cancers that they have. New and different types of therapy are needed to improve survival rates for children with neuroblastoma. Anti-GD2 immunotherapy has already been shown to improve survival for these children, but there is still a lot of work to be done to improve survival rates further.
“Thanks to funding from Niamh’s Next Step, Neuroblastoma UK, and The Bradley Lowery Foundation, I hope the trials I am involved in can build on what has already been achieved, and deliver more effective immunotherapies.”
Funding research. Giving hope.
Tony Heddon, Chair of Neuroblastoma UK says, “Thanks to our generous supporters, we have awarded nearly £7 million to UK research focusing on neuroblastoma. But more needs to be done. We rely on donations to continue to drive forward research into this terrible disease and give more families hope.”
Chris Curry, Niamh’s dad, Co-Founder and Chair of Niamh’s Next Step says, “Having collaborated on various neuroblastoma research projects over the last six years, we are very proud and excited to be working alongside Neuroblastoma UK and The Bradley Lowery Foundation to fund this project run by Dr Gray in Southampton. It’s amazing to continue funding vital projects like this in Niamh’s memory.”
Gemma Lowery, Bradley’s mum and founder of The Bradley Lowery Foundation says, “The Bradley Lowery Foundation believe collaborating with other like-minded charities and organisations is the best way to achieve the goals you desire. Working with so many great charities, we have been able to support vital research into neuroblastoma, in the hope that one day, it can be cured for good. BLF are honoured to join Neuroblastoma UK and Niamh’s Next Step in funding this research and we believe, together, great things can be achieved.’’